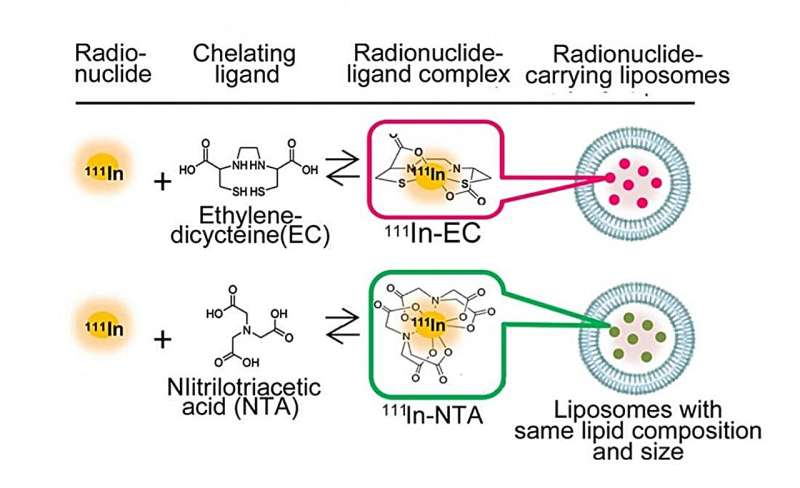
Figure 1. The radionuclide-encapsulated liposomes, including the focus of the study, a ligand called ethylenedicysteine (EC). Credit: Umeda et al
A team of researchers has developed a new method that suppresses the distribution of drugs to healthy tissues and also rapidly removes the drugs once distributed in the body, which could improve the accuracy of imaging diagnosis of difficult cancers, reduce toxicity to healthy tissues, and further improve the effectiveness of treatment. They report their findings in a recent study published in the Journal of Controlled Release.
Radiopharmaceuticals have been attracting attention as the next generation of cancer imaging and cancer treatment drugs. Until now, most research has focused on developing the technology to deliver drugs to cancer lesions, but it has been impossible to avoid distributing drugs to healthy tissues.
A team of researchers, led by National Cancer Center Exploratory Oncology Research & Clinical Trial Center Functional Diagnostics Development Field researchers Izumi Umeda, who at the time was also a Project Researcher at the Kavli Institute for the Physics and Mathematics of the Universe (Kavli IPMU), and Hirofumi Fujii, alongside researchers from Chiba University, Kavli IPMU, and Kyoto College of Medical Science, combined components in nuclear medicine, drug delivery systems (DDS) and complex chemistry to develop a method that controls the in vivo dynamics of radionuclides post-administration.
The team's method allows radiopharmaceuticals to accumulate sufficiently in cancer lesions, while shortening the time the drugs are in contact with healthy tissues. This means drugs can concentrate on the cancer lesions, improving their effects compared to conventional methods.
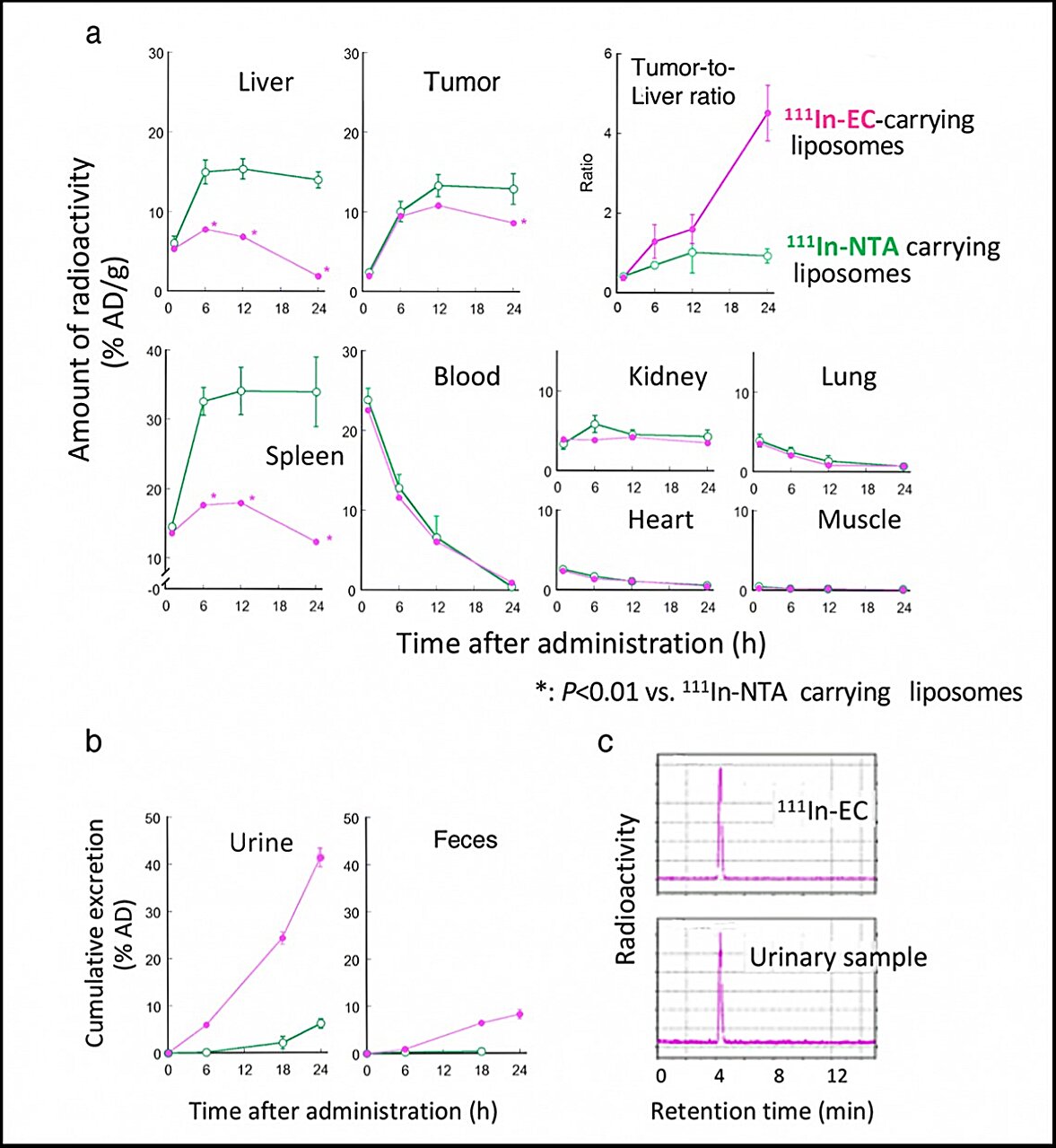
Figure 2. Time-dependent biodistribution of 111In-radioactivity in tumor-bearing mice after administration of 111In-EC- and 111In-NTA-carrying liposomes. (a) shows time-dependent uptake, retention, and clearance of 111In radioactivity in each organ and tumor, while (b) shows accumulated excretion of 111In radioactivity with time in the urine and feces. (c) HPLC analysis of radioactive material in urine. Credit: Umeda et al
The two types of radiopharmaceuticals, or RI-encapsulated liposomes (Figure 1), have the same liposome composition and particle size, and the RI is the same 111In, differing only in the ligand. Nitrilotriacetic acid (NTA) is a typical ligand, and ethylenedicysteine (EC) is the new ligand at the center of the team's experiment.
Two types of 111In-ligand-containing liposomes were given to mice with tumors, and researchers monitored the uptake and accumulation of 111In in cancer and healthy tissues, especially the liver and spleen (Figure 2). There was little difference in the tumors in both mice, but in the liver and spleen, 111In-EC-liposomes were once taken up but then rapidly cleared out, whereas conventional 111In-NTA-liposomes remained for a long time. The 111In-EC-liposomes also promoted excretion into feces, and the chemical form in urine was 111In-EC not in the liposomes.
The team found that in the liver, the liposomes were broken up, releasing the 111In-ligand complexes inside, whereas in the tumor, liposomes persisted intact for a long time and the 111In-ligand complexes remained in liposomes. The unique complex, 111In-EC, allowed for rapid clearance from the liver after being released from the liposomes.
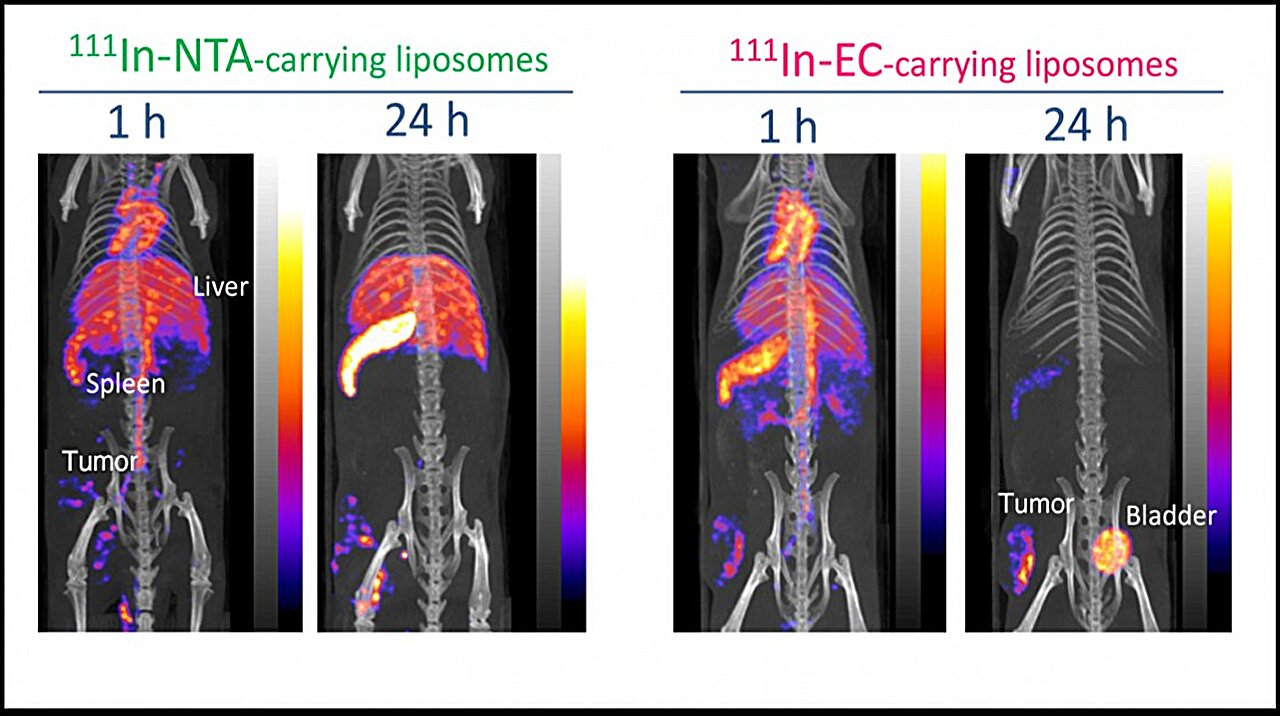
Figure 3. In vivo SPECT/CT images of the two types of 111In-carrying liposomes in-tumor-bearing mice at 1 and 24 h after administration. Credit: Umeda et al
In the in vivo SPECT/CT images of tumor-bearing mice after administration of 111In-EC- or 111In-NTA-liposomes (Figure 3), the distribution of the two liposomes in the body was almost identical to begin with. However, later, the 111In-EC-liposomes appeared clearly in tumor sites due to a negligible signal from the liver and spleen, whereas 111In-NTA-liposomes were unable to selectively image tumors due to their low clearance from the above organs. The images were consistent with the biodistribution studies described above.
Based on the results of this study, the team proposed a scheme explaining the in vivo fate of radionuclide-carrying liposomes (Figure 4). After intravenous administration, conventional 111In-NTA-liposomes and new 111In-EC-liposomes circulate in the bloodstream and accumulate to a similar extent in tumors. Most liposomes remain intact within the tumor for a long time, and consequently, the encapsulated radionuclide-ligand complexes are retained within liposomes. Furthermore, liposomes are taken up by the liver, where they are rapidly degraded and release their encapsulated 111In-ligand complexes.
After their release from liposomes, conventional 111In-ligand complexes, such as 111In-NTA, remained in the liver for a long time. In contrast, 111In-EC were able to escape from the liver and were rapidly excreted in the urine in its original form. The researchers say rapid urinary excretion without accumulation in other tissues will allow radioactivity to be cleared swiftly from the body and minimize damage.
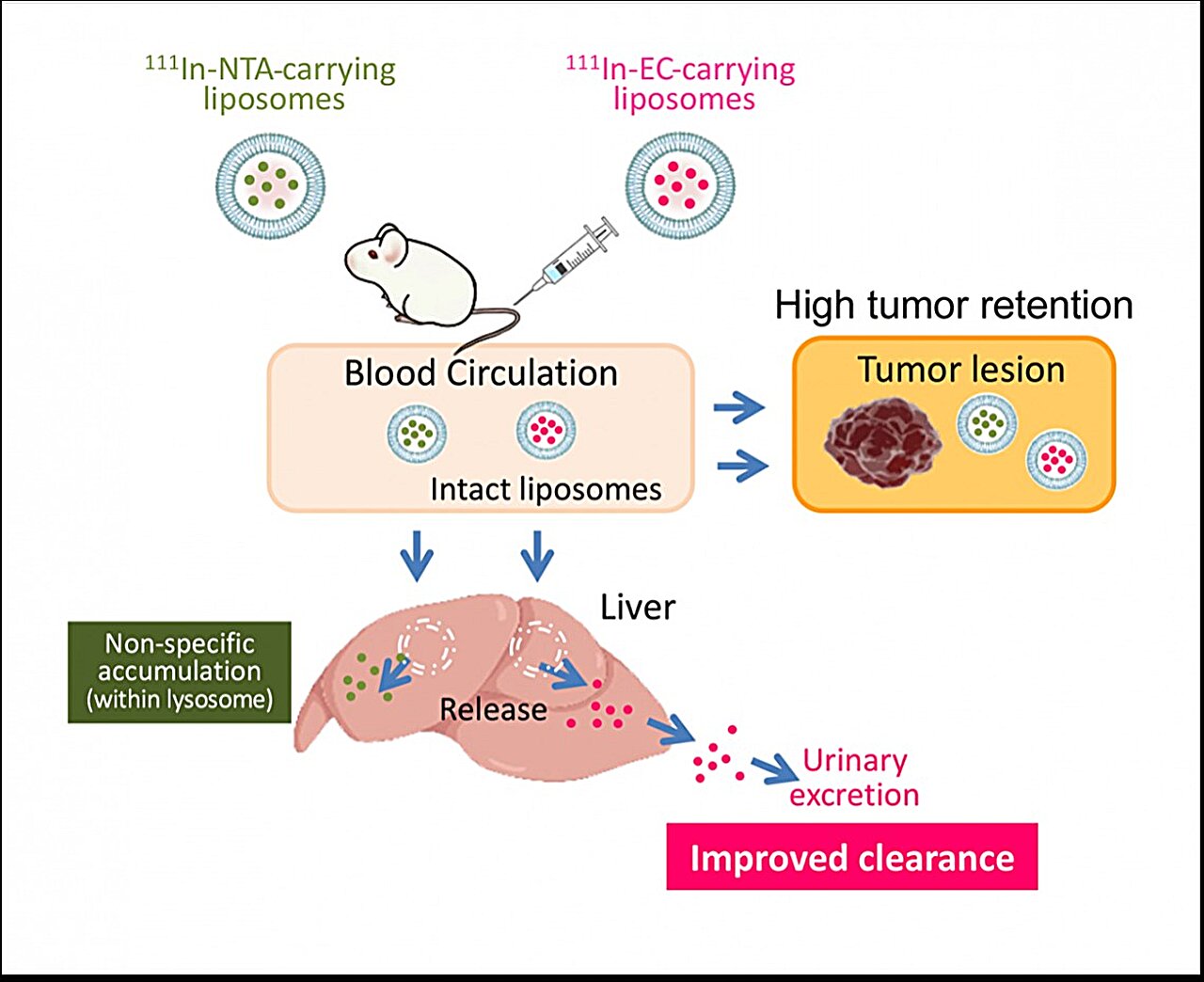
Hypothesized in vivo fate of radionuclide-carrying liposomes in tumor-bearing mice. Credit: Umeda et al
"The fact that a new approach to drug development has been developed at this time from a new perspective to maintain the concentration of drugs in cancer lesions while protecting healthy tissue is important when considering the role high-precision cancer treatment, or theranostics, will play in the treatment of the intractable. In the future, we hope that further research will lead to drugs that stay only in cancer lesions, which has never been done before," said Umeda.