A novel PET imaging tracer has been proven to safely and effectively detect a common cancer gene mutation that is an important molecular marker for tumor-targeted therapy. By identifying this mutation early, physicians can tailor treatment plans for patients to achieve the best results. This research was published in the December issue of The Journal of Nuclear Medicine.
Kirsten rat sarcoma (KRAS) is a commonly mutated oncogene that is present in approximately 20-70 percent of cancer cases. Patients with KRAS mutations usually respond poorly to standard therapies. As such, the National Comprehensive Cancer Network and other leading cancer research centers recommend assessing the mutation status in cancer patients to determine the most effective treatment.
“Currently, KRAS mutation screening relies on a biopsy combined with gene sequencing. However, biopsies have the potential for significant complications and their use is limited by the quality of the tissue sample. Thus, there is an urgent need for accurate yet noninvasive methods of evaluating the KRAS mutation status,” stated Jing Wang, MD, PhD, nuclear medicine physician at Xijing Hospital of Fourth Military Medical University in Xi’an, China.
In this first-in-humans study, researchers sought to develop a KRAS-targeted radiotracer and investigate its targeting potential in non-small cell lung cancer (NSCLC) and colorectal cancer.
An oncoprotein-targeted PET tracer, 18F-PFPMD, was created based on a recently FDA-approved KRASG12C inhibitor. The targeting specificity and imaging ability of the tracer were assessed through both in vitro and in vivo study. Further evaluation in healthy volunteers, non–small cell lung cancer (NSCLC) patients, and colorectal cancer (CRC) patients was also conducted.
18F-PFPMD was obtained with a high radiochemical yield, radiochemical purity, and stability and was proven to selectively bind to the KRASG12C protein in preclinical studies. The tracer was found to be safe for humans, clearing rapidly from the gallbladder and intestines. In NSCLC and colorectal cancer patients, 18F-PFPMD accumulation was significantly higher in tumors with the KRASG12C mutation as opposed to those without the mutation.
“This research reveals that 18F-PFPMD is a promising molecular imaging tool of significant clinical relevance,” said Wang. “Moving forward, the tracer could be useful to screen the KRASG12C mutation status, as well as for patient selection of KRASG12C targeted therapy. Moreover, it could be used for monitoring therapeutic response and drug resistance for cancer patients.”
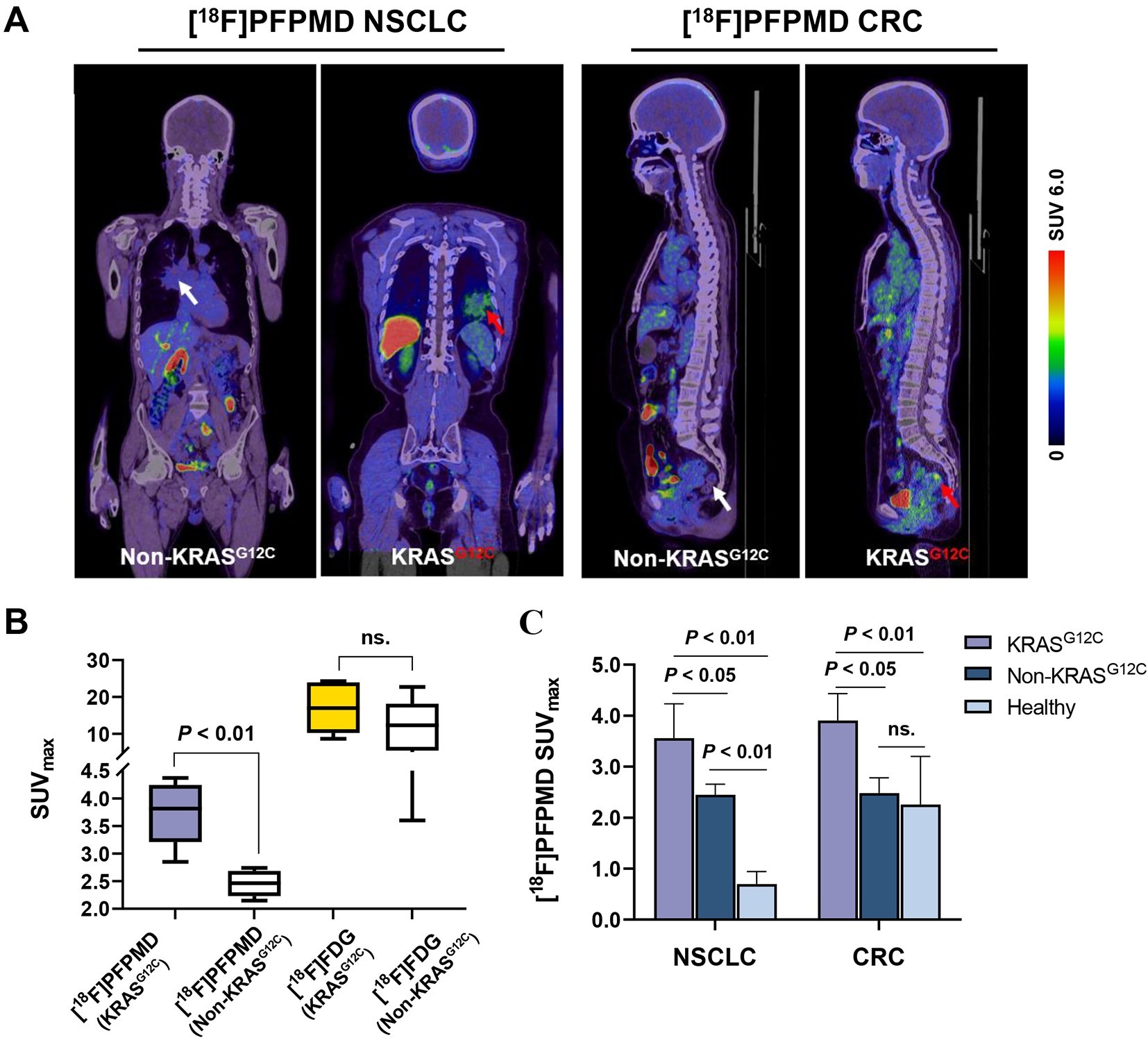
Figure 5. 18F-PFPMD PET/CT imaging of NSCLC and CRC patients. (A) Representative 18F-PFPMD PET/CT images of non-KRASG12C and KRASG12C tumors in NSCLC and CRC patients, respectively. (B) SUVmax of 18F-PFPMD and 18F-FDG in non-KRASG12C and KRASG12C tumors, respectively (KRASG12C, n = 6; non-KRASG12C, n = 8). (C) 18F-PFPMD SUVmax of non-KRASG12C tumors, KRASG12C tumors, and healthy tissue in NSCLC patients, CRC patients, and healthy volunteers, respectively (NSCLC: KRASG12C, n = 3; non-KRASG12C, n = 5; healthy, n = 5) (CRC: KRASG12C, n = 3; non-KRASG12C, n = 3; healthy, n = 5). ns = not statistically significant.