PET scans typically used for diagnosing prostate cancer may have value in detecting inflammatory bowel disease (IBD), according to a case series published December 8 in Clinical and Experimental Gastroenterology.
In the study, PET/CT imaging with F-18 DCFPyL radiotracer -- a PET tracer approved for diagnosing suspected prostate cancer relapse -- effectively revealed regions of inflamed intestinal mucosa in patients with active IBD, according to lead author Mohamed Saleh Ismail, MD, of Johns Hopkins University in Baltimore, MD, and colleagues.
“The ability to accurately and noninvasively detect and monitor gastrointestinal inflammation in IBD patients would have broad clinical impact by contributing to therapeutic management decisions,” the group wrote.
Inflammatory bowel disease (IBD) is a chronic inflammatory condition of the gastrointestinal tract characterized by remission and relapse. There is no single test available that can accurately detect asymptomatic inflammation in these patients, the researchers wrote.
However, recent studies have shown that prostate-specific membrane antigen (PSMA) is minimally expressed in the normal gastrointestinal tract but is highly and specifically upregulated in inflamed endoscopic biopsies of both Crohn’s disease and ulcerative colitis patients, they added.
Thus, to test whether PSMA-PET may be effective in patients with IBD, the group performed F-18 DCFPyL (Pylarify, Lantheus Medical Imaging) PET/CT imaging in three patients with active disease -- two with Crohn’s disease and one with ulcerative colitis.
In all patients, abnormally increased gastrointestinal F-18 DCFPyL uptake was observed in areas with endoscopic, histologic, and immunohistochemical inflammation, demonstrating partial overlap of segments of bowel with abnormal tracer uptake and active inflammation, according to the findings.
In the ulcerative colitis case, for instance, a 66-year-old man presented to the emergency department with symptoms of flare, including bloody diarrhea of more than 30 bowel movements per day, urgency, and abdominal pain. He was admitted to the hospital.
The patient underwent a flexible sigmoidoscopy to 20 cm from the anal verge, which demonstrated spontaneous bleeding and ulcerations throughout the examined mucosa, according to the report.
A subsequent PET/CT exam demonstrated abnormally increased F-18 DCFPyL uptake in the descending colon, sigmoid colon, and rectum in a distribution corresponding to the findings on endoscopy, the authors wrote.
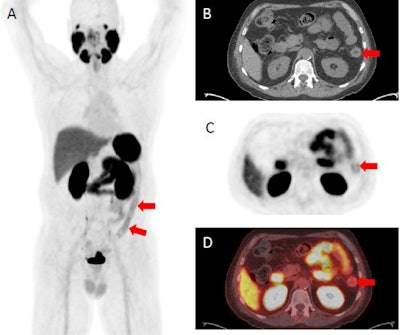
F-18 DCFPyL PET/CT demonstrating abnormally increased uptake in the descending colon (identified by red arrows), sigmoid colon, and rectum corresponding to findings on endoscopy. (A) F-18 DCFPyL PET/CT uptake in the descending colon on a coronal plane. (B) Axial CT image with arrows identifying active inflammation in the descending colon. (C) Axial PET imaging arrows identifying active inflammation in the descending colon. (D) Axial F-18 DCFPyL PET/CT fusion imaging identifying active inflammation in the descending colon. Image courtesy of Clinical and Experimental Gastroenterology.
Ultimately, the accurate and noninvasive diagnosis of active mucosal inflammation in patients with known IBD is a clinical challenge, as there is no single noninvasive gold standard test, biomarker, or imaging agent to reliably diagnose inflamed mucosa during a flare or to monitor disease activity after treatment is initiated, the authors noted.
“This study demonstrates that PSMA-targeted F-18 DCFPyL PET can effectively detect regions of inflamed mucosa in patients with IBD, suggesting its utility as a noninvasive imaging agent to assess location, extent, and disease activity,” the group concluded.