PET imaging with 68Ga-FAPI can more effectively detect and stage pancreatic cancer as compared with 18F-FDG imaging or contrast-enhanced CT, according to new research published in the December issue of The Journal of Nuclear Medicine. In a head-to-head study, 68Ga-FAPI detected more pancreatic tumors on a per-lesion, per-patient, or per-region basis and led to major and minor changes to clinical management of patients. In addition to enhancing precise detection of pancreatic cancer, 68Ga-FAPI imaging also paves the way for future targeted radiopharmaceutical therapies.
Approximately 64,000 Americans are diagnosed with pancreatic cancer each year. The disease is often diagnosed in advanced or metastasized stages and, as a result, is associated with extremely poor survival.
“Existing diagnostic approaches and workups are not sufficient for early detection of pancreatic cancer in curative stages for most patients,” said Jens T. Siveke, MD, translational and GI oncologist of the German Cancer Consortium (DKTK) at the West German Cancer Center in Essen, Germany. “Consequently, there is a pressing need for earlier and more precise disease detection, as well as a demand for novel targeted therapies.”
Recent studies have demonstrated high radiotracer uptake of 68Ga-FAPI in pancreatic cancer lesions; however, the precise diagnostic accuracy and the correlation of the tracer remain unexplored. In this study researchers sought to provide comprehensive data on the diagnostic performance of 68Ga-FAPI in pancreatic cancer patients.
Sixty-four patients with suspected or proven pancreatic cancer were included in the study. All patients underwent 68Ga-FAPI PET and contrast-enhanced CT, and 38 of the patients also underwent 18F-FDG PET. Researchers observed the association of the 68Ga-FAPI PET uptake intensity and histologic FAP (fibroblast activation protein) expression. The detection rate, diagnostic performance, inter-reader reproducibility, and change in management were also analyzed.
The association between 68Ga-FAPI PET uptake intensity and FAP expression was found to be significant, and 68Ga-FAPI PET showed high sensitivity and positive predictive values. In a head-to-head comparison with 18F-FDG and contrast-enhanced CE, 68Ga-FAPI PET detected more tumors on a per-lesion (84.7 vs. 46.5 vs. 52.9 percent), per-patient (97.4 vs. 73.7 vs. 92.1 percent), or per-region (32.6 vs. 18.8 vs. 23.7 percent) basis, respectively. 68Ga-FAPI PET readers showed substantial overall agreement, and minor and major changes in clinical management occurred in nearly 10 percent of patients after 68Ga-FAPI PET.
“Our research suggests that 68Ga-FAPI could become a building block in the diagnostic work-up of pancreatic cancer to improve early detection and accurate staging of this disease,” noted Lukas Kessler, MD, resident in the Department of Nuclear Medicine at University Hospital Essen in Germany. “Furthermore, our results support further investigation of FAP as a potential theranostic target of the tumor microenvironment, which represents an exciting new avenue in combating this enigmatic and fatal disease.”
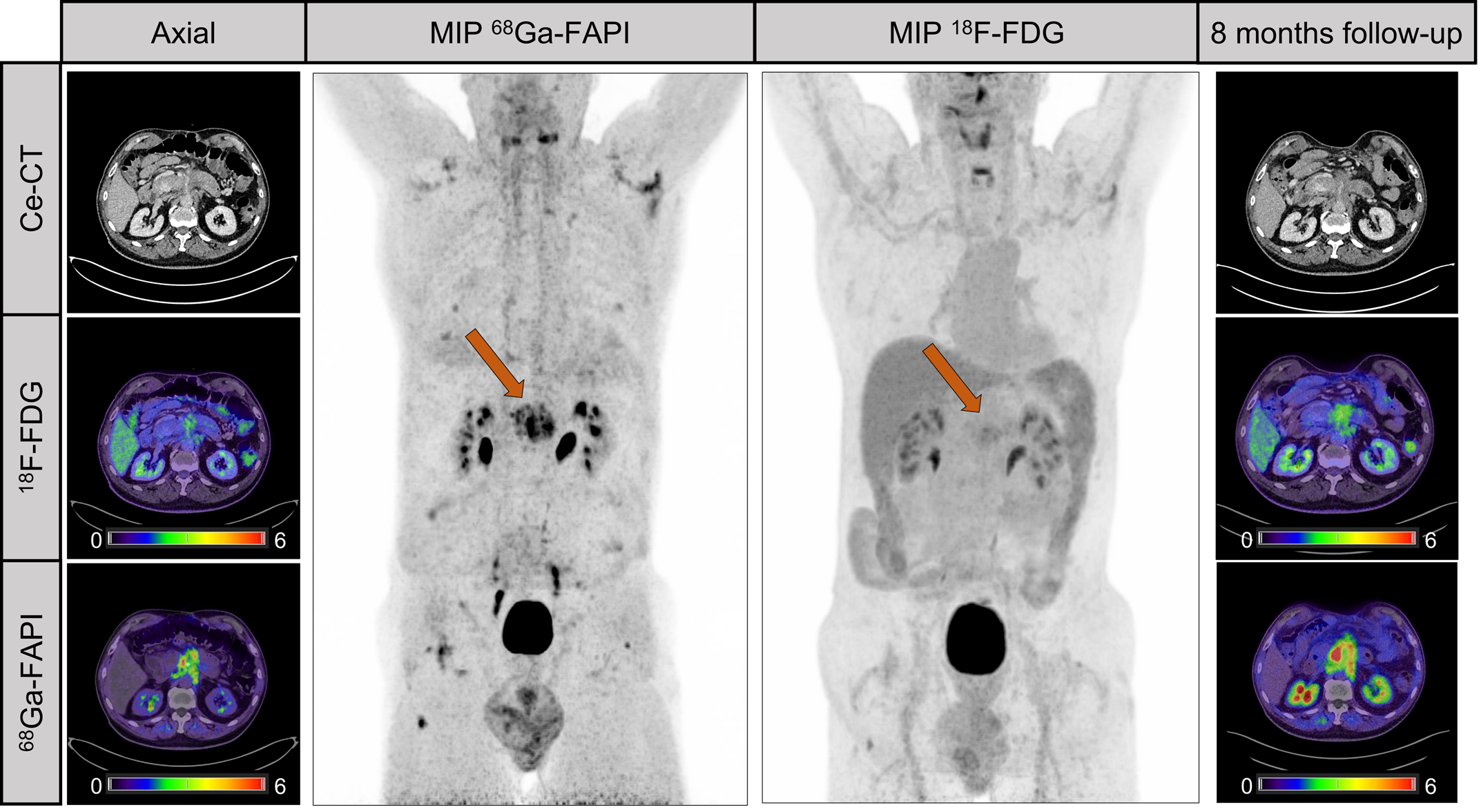
Figure 3. Case presentation. Male patient with suspected recurrent pancreatic cancer. Ce-CT shows mass around superior mesenteric artery after pancreatectomy. 18F-FDG only shows discrete uptake of lesion (SUVmax, 3.8), whereas 68Ga-FAPI clearly visualizes recurrent tumor. Patient received adjuvant chemotherapy after 68Ga-FAPI. Patient denied recommended chemotherapy. Increase of CA19-9 levels (from 240 to 767 U/mL) and follow-up imaging 8mo later validated progression of mesenteric mass as well as increased 18F-FDG uptake (SUVmax, 5.3). MIP 5 maximum-intensity projection.